What is Nerve Pain
How it Affects Health | How to Treat | How to Use StimOn | Why StimOn
Basic Information
Nerve pain (neuralgia), also known as neuropathic pain, occurs when there is damage to or dysfunction of the nervous system. It often presents as a shooting, stabbing, or burning sensation. This type of pain can result from various conditions, including diabetes, injuries, infections, or neurological disorders.1
Chronic Pain, Post-surgical or Post-traumatic Pain
Chronic pain is a type of pain that persists for an extended period, typically defined as lasting longer than three to six months. It can be nociceptive (related to tissue damage), neuropathic (due to nerve damage), or a combination of both. Unlike acute pain, which serves as a protective mechanism and typically resolves with healing, chronic pain can occur without a clear cause and may persist even after an injury has healed. It can be managed in various ways within the field of medicine. On a smaller scale, methods such as regular exercise, physical therapy, and meditation may offer relief. However, these approaches might not be sufficient for patients experiencing significant chronic pain, such as that following surgery or a traumatic event.2

Credit: Image retrieved from West Pompano Pain
Chronic Pain Cycle
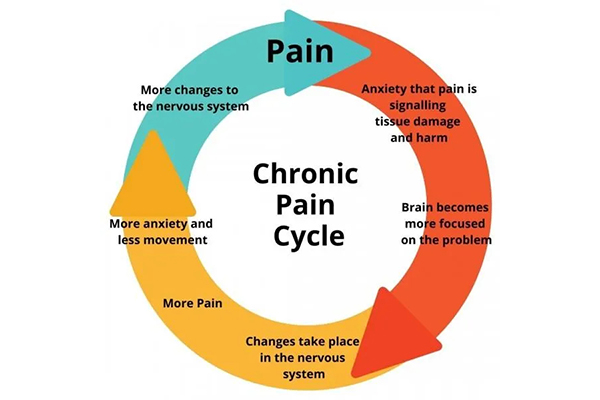
Even after an initial injury has healed, the brain can "learn" to experience pain. Sensations or movements from the previously injured area may trigger anxiety about potential damage. This heightened awareness can lead to changes in neural pathways, causing the brain to interpret sensations as more painful, even when there’s no actual harm. Increased pain leads to more anxiety and reduced movement, creating a cycle of progressive deconditioning and further sensitivity in the nervous system. In essence, the brain's pathways can rewire to become more sensitive to sensations and movements, as shown in the diagram on the left.3
Pain Theory
Pain theory encompasses various scientific viewpoints that explain how we perceive and experience pain. Here are some of the main theories: 4
Gate Control Theory: Proposed by Melzack and Wall, this theory suggests that spinal "gates" regulate pain signals, with non-painful stimuli capable of closing these gates and reducing pain perception.
Specificity Theory: This theory suggests that specific nerve fibers transmit pain signals, linking stimulus intensity directly to pain levels.
Biopsychosocial Model: This approach incorporates biological, psychological, and social factors, emphasizing that pain is influenced by emotional and contextual elements, not just physical sensations.
Neuro-matrix Theory: Developed by Melzack, this theory views pain as a complex experience arising from a network of brain regions that integrate sensory, emotional, and cognitive inputs.
In clinical settings, Gate Control Theory is frequently referenced, particularly in physical therapy and pain management, as it illustrates how non-painful stimuli can help reduce pain. Understanding the nerve pain pathway and its various stages is important, as grasping this concept is crucial for effectively controlling and managing pain.4
Nerve Pain Pathway
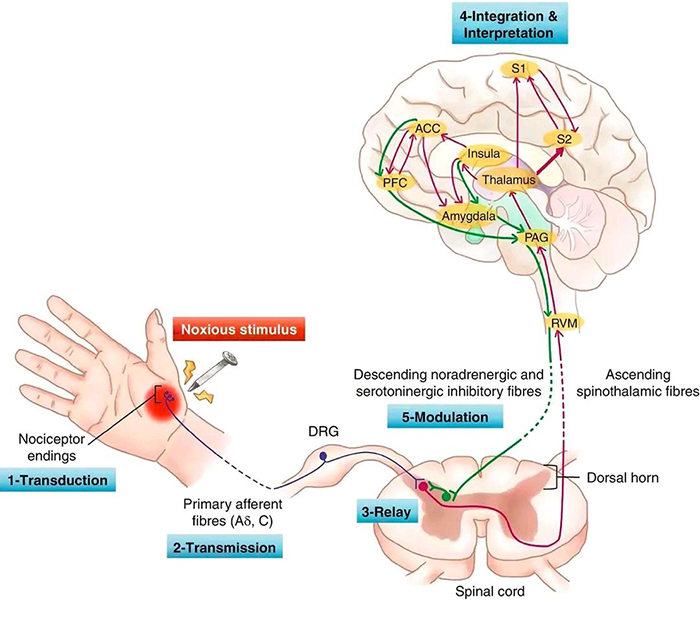
The pathway of nociceptive pain consists of several stages: 5
- Transduction (Detection of Noxious Stimulus): Nociceptors in tissues (e.g., skin, muscles, organs) detect harmful stimuli (e.g., heat, pressure) and convert them into electrical signals (action potentials).
- Transmission (Signal Relay to the Spinal Cord): The electrical signal travels through afferent nerve fibers (e.g., A-delta or C fibers) to the spinal cord, entering through the dorsal horn.
- Relay (Transmission to the Spinal Cord): The pain signal is relayed to second-order neurons in the spinal cord, where it can be modified, amplified, or suppressed before being sent to the brain.
- Integration & Interpretation (Brain Processing and Awareness): The signal reaches the thalamus and somatosensory cortex, where it is processed for location, intensity, and quality. The brain perceives pain as a conscious sensation.
- Modulation (Pain Regulation and Response): The brain can activate descending pathways (e.g., from the rostral ventromedial medulla) to regulate pain at the spinal cord level, using inhibitory neurotransmitters like serotonin and endorphins to reduce pain perception.
The diagram below highlights the complexity of pain as a sensory experience, outlining the stages of nociceptive pain.6
Credit: Image retrieved from Pathophysiology of Pain
Reference :
- Healthdirect. (n.d.). Nerve pain (neuralgia).
- Ryan. (2021). Chronic pain: A complete analysis. Wellness and Health Tips.
- Capital Area Physical Therapy & Wellness. (n.d.). Chronic Pain and Physical Therapy: The Role of Physical Therapy in Chronic Pain Management.
- Physiopedia. (n.d.). Theories of pain.
- Osterweis, M., Kleinman, A., Mechanic, D. (1987). Pain and Disability: Clinical, Behavioral, and Public Policy Perspectives. Washington (DC): National Academies Press.
- Martin, E. (2018). Pathophysiology of Pain. Pain Management in Older Adults. Cham, Switzerland: Springer.